Temporomandiubular Joint Physiotherapy (Jaw Physio)

Anatomy
The temporomanidbular joint (TMJ) is made up of the mandibular fossa on the temporal bone (skull side), an articular disc (piece of cartilage), the retrodiscal tissue (connective tissue) and the mandible condyle (jaw side). The joint acts like a sort of sliding hinge which allows protrusion (underbite), retraction/retrusion (overbite), deviation (side to side) as well as jaw opening and closing. You can feel this joint move if you put your index finger just in front of the middle your ear and open/close, protrude or deviate the jaw.
The articular disc is a biconcave (peanut shape) disc that sit’s between the two articular surfaces (fossa and condyle). Its role is to act as a stress absorber for the jaw and displace the mandibular condyle (bottom bit) from the mandibular fossa (top bit) to allow movement of the jaw.
The retrodiscal tissue acts as an anchor for the articular disc, preventing it from being pulled forward when the jaw opens and remain in its correct position. It is also highly innervated and can be a source of pain.
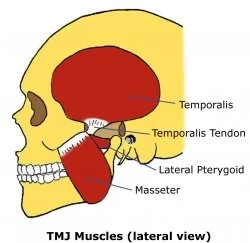
The primary muscles of mastication (eating) are the temporalis muscles, the masseter muscles and the pterygoid muscles. The temporalis muscles control the up and down jaw movements whilst the pterygoids control deviation and protrusion/retraction.
The nerve that supplies these muscles and sensation for the face is cranial nerve V, the Trigeminal nerve.
TMJ Dysfunction
Temporomandibular dysfunction (TMD) is an umbrella term for some conditions that cause jaw pain. Below are a list of common causes.
Clenching
Jaw pain may be caused by mouth habits like clenching, chewing (e.g. gum) or bruxism (grinding). These people have unconscious habits that ramp up muscle activation of their temporalis and masseter muscles. These habits cause excessive squeezing of the articular disc and retrodiscal tissue resulting in jaw pain. The muscle activation can also present as temporal, tension type headaches.
To test if you’re a clencher you can simply place your hands over the temporalis muscle and clench your jaw slightly. If you feel big bulging muscles push into your hands you’re probably a clencher. If they’re not so big, you’re probably not. If you’re unsure, ask your partner or a friend if you can feel their temporalis muscles to compare.
Treatment for clenching is pretty simple, stop clenching. Be aware of your mouth posture, resting posture should be lips together, teeth apart. Some patients will be given stretches to do to help the muscles to relax if beneficial for pain. Some may be referred to a dentist for a night splint.
Internal Derangement
Internal derangement is an articular problem of the TMJ. It relates to the disc and its position during resting and mouth opening/closing. The likely cause of internal derangement is trauma or long term clenching and grinding.
This disorder has 4 sub categories.
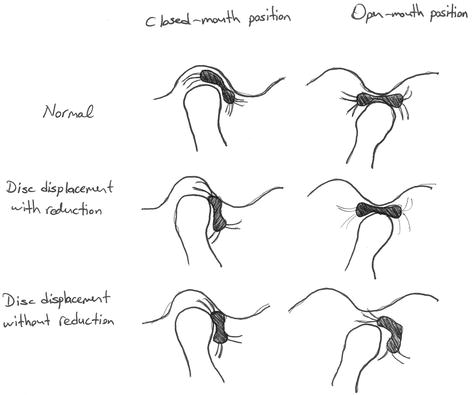
Disc displacement with reduction. The articular disc is displaced anteriorly (forward) at rest, when the mouth is opened the disc relocated onto the condylar head. These patients may have a click during opening. Protrusion usually stops this click. They have little or no reduction in range. This is typically associated with a deviation (middle-out-middle) during opening as the disc reduces.
Disc displacement with reduction with intermittent locking. As above, however the disc may occasionally not relocate, resulting in occasional locking.
Disc displacement without reduction with limited opening. The disc does not reduce during opening, preventing the jaw from being opened very far. This is associated with jaw pain and occasional clicking and popping. Jaw opening is typically limited to < 40mm. This is typically associated with a deflection (middle-out-further out).
Disc displacement without reduction without limited opening. These patients did fit into category 3 at some point. Now, the disc has “worn out” and they no longer have limited opening and are usually now pain free.
Physiotherapy treatment for internal derangement is typically for pain relief, we cannot relocate the disc. This may be in the form of mobilisations of the jaw. In severe cases, patients may seek corticosteroid injections or a surgical opinion.
Trigeminal nerve irritation
Other symptoms that are common with TMD include one weepy eye, one drippy notril or face dysthesia. The weepy eye or drippy nostril may be a result of Trigeminal nerve irritation resulting in a ramping up of parasympathetic outflow. Facial dysthesia (loss of sensation or pins and needles) is likely due to a compression of the trigeminal somewhere.
Dentists
Dentists, being experts in all things mouth, jaw and teeth, can play a role in diagnosing and treating your orofacial pain. We occasionally refer patients to their dentist for a second opinion or to get a night splint to prevent grinding and clenching at night.
Differential Diagnoses
Trigeminal nerve neuralgia - horrible, shooting, lightning bolt pain facial or jaw pain. The most common cause is idiopathic (no obvious cause, random dumb luck) but it may also be caused by trauma or dental procedure. There are a few cases of people having an artery pressing against their Trigeminal nerve also causing this pain or odd things like a winking eye.
Trigeminal neuritis - as above due to inflammation of the Trigeminal nerve, also idiopathic.
Complex region pain syndrome - pain with no apparent physiological cause, typically secondary to a traumatic event and worsened by anxiety.
Vestibular hypofunction - another cause of headache. Read more about it here.
Headaches need to be differentiatly diagnosed from other causes. You can read about headaches hear.